Diabetic Retinopathy
Diabetic retinopathy can happen to anyone who has type 1 or type 2 diabetes, and according to the National Eye Institute, up to 45 percent of adults diagnosed with diabetes in the United States have some degree of diabetic retinopathy. The longer you have diabetes, the more likely you are to develop diabetic retinopathy.
What are the stages of diabetic retinopathy?
Diabetic retinopathy has four stages:
1. Mild Nonproliferative Retinopathy. At this earliest stage, microaneurysms occur. They are small areas of balloon-like swelling in the retina’s tiny blood vessels.
2. Moderate Nonproliferative Retinopathy. As the disease progresses, some blood vessels that nourish the retina are blocked.
3. Severe Nonproliferative Retinopathy. Many more blood vessels are blocked, depriving several areas of the retina with their blood supply. These areas of the retina send signals to the body to grow new blood vessels for nourishment.
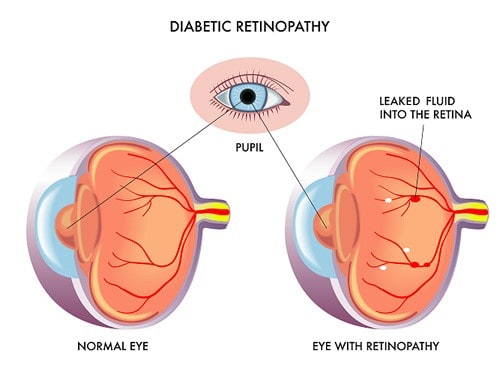
4. Proliferative Retinopathy. At this advanced stage, the signals sent by the retina for nourishment trigger the growth of new blood vessels. This condition is called proliferative retinopathy. These new blood vessels are abnormal and fragile. They grow along the retina and along the surface of the clear, vitreous gel that fills the inside of the eye. By themselves, these blood vessels do not cause symptoms or vision loss. However, they have thin, fragile walls. If they leak blood, severe vision loss and even blindness can result.
Symptoms
Diabetic retinopathy usually affects both eyes. Symptoms can be unusual in the early stages, but as the condition progresses symptoms may include:
- Spots floating in your vision
- Blurred vision
- Poor night vision
- Dark streaks or a red film that blocks your vision
- Vision loss
Risk Factors
The longer you have diabetes, the greater your risk of developing diabetic retinopathy. Diabetic retinopathy can happen to anyone who has diabetes. The risk is highest if you:
- Have high blood pressure
- Have poor control of your blood sugar level
- Have high cholesterol
- Are pregnant
- Smoke
- Are Black or Hispanic
Treatment
During the first three stages of diabetic retinopathy, no treatment is needed, unless you have macular edema. To prevent progression of diabetic retinopathy, people with diabetes should control their levels of blood sugar, blood pressure, and blood cholesterol.
If you have proliferative diabetic retinopathy, you’ll need surgical treatment promptly. For severe nonproliferative diabetic retinopathy, surgery may be recommended and depending on the specific problems with your retina, options may include:
- Focal laser treatment, a laser treatment, also referred to as photocoagulation, can stop the leakage of blood and fluid in the eye. This procedure is done in your doctor’s office or eye clinic. During this procedure, laser burns seal the leaks from abnormal blood vessels. Your vision will be blurry for about a day after the procedure. Sometimes small spots caused by the laser burns may appear in your visual field. However, if you had blurred vision from swelling of the central macula before surgery, you may not recover completely normal vision.
- Scatter laser treatment, also known as panretinal photocoagulation, is a laser treatment that can shrink the abnormal blood vessels and this is also done in your doctor’s office or eye clinic. During the procedure, the areas of the retina away from the macula are treated with scattered laser burns and these burns cause the new blood vessels to shrink and disappear. Your vision will be blurry for about a day after the procedure and it is possible to have some loss of peripheral vision or night vision after the procedure.
- Vitrectomy, is a procedure that can be used to remove blood from the vitreous (the center of the eye) and scar tissue that’s tugging on the retina. This procedure is done in a surgery center or hospital under local or general anesthesia. During the procedure, the doctor makes a tiny incision in your eye. Blood-filled tissue and scar tissue are removed with delicate instruments and replaced with a salt solution, and this helps maintain your eye’s normal shape. You may stay in the hospital overnight after surgery. In some cases, a gas bubble must be placed in the cavity of the eye to help reattach the retina and this can cause a longer stay in the hospital because you may need to remain in a facedown position until the gas bubble disappears which can take several days. Your eye surgeon will instruct you on how to use an eye patch and use medicated eyedrops for a few days or weeks. Vitrectomy is often followed or accompanied by laser treatment.
Although there is no cure for diabetic retinopathy, surgery often slows or stops the progression. It is very important to protect your vision and take prevention seriously. If it has been a year since your last eye appointment, schedule your yearly eye exam with Morristown Ophthalmology Associates, P.A. today.





